Endodontic Therapy

What is endodontic treatment?
The word “endodontic” comes from two Greek words: Endo and odont. Endo means “inside,” and “odont” is Greek for “tooth.” Hence endodontic treatment are procedures that treat the inside of the tooth.
What does the “inside” of a tooth consist of? Inside the tooth is a soft tissue called the pulp. The pulp consists of blood vessels, nerves and connective tissue. It is surrounded by a hard layer called dentin. Overlying the dentin is the white enamel, which forms the crown of the tooth. The crown is supported by the root(s)
The pulp fills the canals inside the roots of the tooth and emerges at the tips of the roots. There the pulp connects with the tissue surrounding the root.
Endodontics is the field of dentistry that deals with diagnosis and treatment of the dental pulp.
When is endodontic treatment necessary?
Endodontic treatment is necessary when the pulp, which consists of nerves, blood vessels and connective tissue inside the tooth, becomes inflamed or infected from one of many causes. Although the most common cause is deep decay, the pulp can become inflamed from a crack in a tooth, numerous restorative procedures or sudden, forceful impact. Traumatic impact may lead to pulpal inflammation and infection even though there is no visual signs of cracking or external damage. Left untreated, pulpal inflammation and infection may lead to pain symptoms and eventually abscess of the tooth.
What are the symptoms or warning signs that endodontic treatment may be needed?
Symptoms or early warning signs include intermittent low grade pain; chronic sensitivity to cold and especially to hot; pain or tenderness to biting; food trapping in and around the tooth; discoloration of a front tooth, especially weeks or months after an accident; gum swelling or gum “pimple” that drains; swelling or tenderness in lymph nodes under the lower jaw; and facial swelling. Very often there may be no symptoms.
Root canals are famous for causing pain. How can I avoid the pain of having root canal treatment?
With the latest in techniques and anesthetics, profound, deep anesthesia can be achieved consistently and predictably. Most patients are pleasantly surprised at how easily and comfortably endodontic treatment can be accomplished in a relatively short time. This is a benefit of technological advancement in the fast growing field of dentistry.
For the first few days after treatment, your tooth may feel sensitive, especially if there was pain or infection before the procedure. This discomfort can be relieved with over-the-counter or prescription medications. Follow your instructions carefully.

Can endodontic treatment save all teeth?
Endodontic treatment focuses on the complete removal of infection from all the canals of the root and the sealing of the canals to prevent further infection. When this is done and the tooth is restored with a crown or filling, the tooth is “saved.” How is this done?
First of all, decay along with inflamed or infected pulp is removed. Then each canal is located with the help of the 3-D CT scan and the operating microscope. The 3-D CT scan not only helps in locating the entry point to the canals but also in anticipating the “twist and turns” of the canal. Thorough debridement (cleaning) and disinfection of the entire length of the canal is essential to success and the elimination of post-operative symptoms and complications. The operating microscope is indispensable to the modern practice of endodontics. It magnifies and illuminates the operating field such that even canals that can escape the human eye can be detected and treated. Success rate is significantly enhanced when the dentist has the knowledge, experience and skill to use and operate the CT scan and the operating microscope. After every possible canal is located, and its length measured, vis-à-vis the CT scan and electronic canal-measuring devices, then each canal is thoroughly cleaned and shaped with specially designed endodontic files. These files must trace the “twist and turns” of the canals so that all the infected tissue in the canals can be removed. To further ensure complete debridement (cleansing) of the canals, sodium hypo-chloride or other disinfectants are used to “rinse” or irrigate the canals. Additionally, a erbiumYag laser may be used to further complete the disinfection process, after which each canal is filled. A crown or other restoration is needed to restore the tooth to its original shape and function. If decay is extensive, a endodontic post, or a reinforcing pin, may be necessary to help restore lost tooth structure prior to the fabrication of the crown.
Endodontic Procedure
Before any endodontic procedure is recommended, there first must be a complete and thorough diagnosis. Diagnosis is established in four steps.
1. Subjective history. Patient’s symptoms and history of pain is reviewed. Location and nature of pain is noted. The patient may be asked some of the following questions: How long have the symptoms been present? Has the tooth been sensitive to cold and hot liquids? If especially sensitive to hot, inflammation in the pulp may be irreversible. Is the tooth sensitive to chewing pressure? Is the pain at a particular site or is it diffused? Has the patient experienced sinusitis? What procedures have been done in past on this tooth?
2. Objective History. Medical and dental records, where available, are viewed. Relevant medical conditions are identified and physician consultation may be initiated, when appropriate. Previous dental x-rays or records are reviewed. Patient’s health form is thoroughly examined and follow-up questions are asked. Patient’s concerns regarding pain are addressed, especially regarding anesthetics and possible desire for oral, nitrous or IV sedation. History and reaction to anesthetics are reviewed
3. Assessment. Assessing the condition of the tooth is performed in three steps. (a) Clinical information is gathered through questions such as the following: What is the condition of the tooth? How extensive is decay? Are other adjacent teeth also decayed? Is it possible other teeth are contributing to the symptoms? Does the tooth react to cold or hot stimulus, or percussion (gentle tapping)? If pain is diffused, is there sinus involvement? Is the root in proximity of nerves or sinuses that can refer pain? Is the jaw joint (TMJ) normal and functional? How does the tooth occlude (bite) against other teeth? Can a simple bite adjustment of the tooth take care of the problem?
(b) X-rays. Two types of x-rays are now used in dentistry, besides the traditional x-ray taken with film. Digital x-rays are taken with specially designed “sensors” which are up to 10 times more sensitive radiation than film. Hence digital x-rays reduced significantly the amount of radiation needed to procure an image of the tooth. Additionally the computerized images can be enhanced so that even more information can be procured from the x-ray images than film. For example, these images can be enlarged, colorized and textured to give more information.
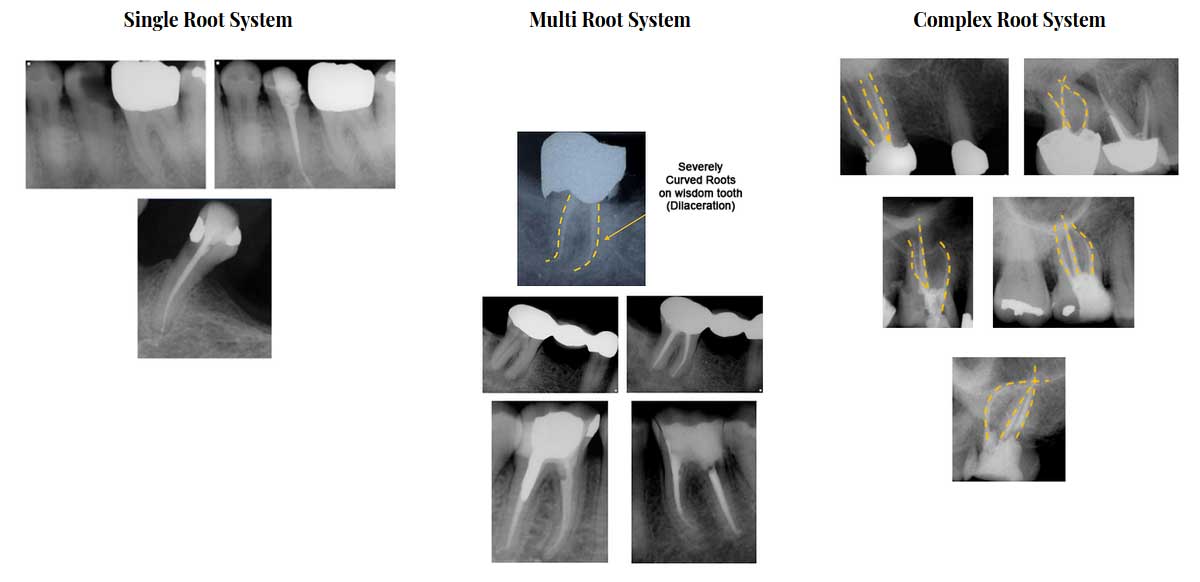
(c) Cone-beam computerized tomography is also used to good effect for imaging configuration of roots and canals. Whereas digital x-rays are two dimensional, CT scans are three dimensional. The latter can reveal abscess formation that can escape two-dimensional x-rays. Bending (dilacerations) of the roots are seen when the 3-D images are turned in various directions. Accessory (branch) canals can often be located more predictably with CT scans. Armed with the cone-beam CT the dentist can more confidently and predictably diagnose and treat endodontic conditions more than ever.
4. Plan/Procedure: Once the diagnosis has been established as described above, then a thorough discussion with the patient is necessary. If the tooth is abscessed, all the reasonable alternatives are brought to the patient’s attention. The alternatives are extraction and replacement with a bridge, partial denture or implant or endodontic treatment. Should the patient elect to undergo endodontic treatment, the prognosis (predictability of success) is discussed. Probable complications are discussed and consent is obtained.
The Steps of the Endodontic Procedure are as follows

Step one: The procedure begins with the administration of the selected local anesthetic.
A rubber sheet called the rubber dam, is placed over the tooth. The rubber dam prevents contamination of the tooth from oral fluids as well as medications or fine instruments from falling out of the field of operation.
Plumber chamber and root canals cleaned and shaped.
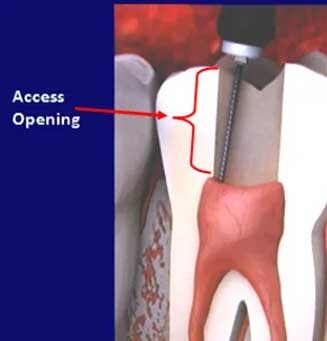
Step two: An opening is made in the crown of the tooth. Very small files and are used to clean the pulp from the pulp chamber and root canals and to shape the space for filling.
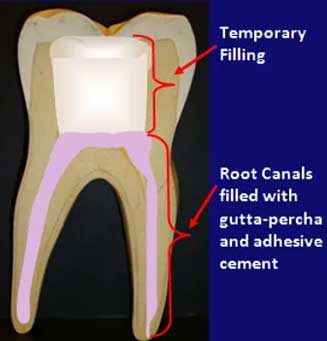
Step three: After the space is cleaned and shaped, the root canals are filled with a biocompatible material, usually a rubber-like material called “gutta-percha.” The gutta-percha is placed with an adhesive cement to ensure complete sealing of the root canals. In most cases, a temporary filling is placed to close the opening. The temporary filling will be removed before the tooth is restored.

Step four: After the final visit a crown or other restoration must be placed on the tooth to protect and restore it to full function.
POST: If the tooth lacks sufficient structure to hold the restoration in place, your dentist or endodontist may place a post inside the tooth. Ask your dentist or endodontist for more details about the specific restoration planned for your tooth
What does root canal treatment cost?
The cost varies depending on how complex the problem is and which tooth is affected. Molars are more difficult to treat, the fee is usually more. Most dental insurance policies provide some coverage for endodontic treatment.
Generally, endodontic treatment and restoration of the natural tooth are less expensive than the alternative of having the tooth extracted. An extracted tooth must be replaced with a bridge or implant to restore chewing function and prevent adjacent teeth from shifting. These procedures tend to cost more than endodontic treatment and appropriate restoration. With root canal treatment you save your natural teeth and money.
What other procedure is needed after endodontic treatment?
A crown or restoration is generally needed to restore the internal portion of the tooth that was removed during the endodontic procedures. Where the decay was extensive, an endodontic post may be needed to provide the crown sufficient retention. New trauma, deep decay, or a loose, cracked or broken filling can cause new infection in your tooth.