Cowards Welcome
COWARDS OR HIGHLY SENSITIVE PATIENTS ARE ESPECIALLY WELCOME AT ALHAMBRA DENTAL. Technological advances in dental anesthesiology have been integrated into Dr. Chao’s patient care, so that even the most sensitive and anxious patients, in a short time, actually look forward to and enjoy their visits with us. Total patient ease and comfort is the central theme of our practice. This theme extends to the way our staff answers your first call, the way you are warmly greeted, to the professionalism used to communicate with you regarding your needs and concerns.
OVERCOME DENTAL PHOBIA THROUGH IATROSEDATION®
By John Chao, DDS, MAGD
Faculty, Behavior Science Section
USC School of Dentistry
Since 1974 thousands of fearful patients have been successfully treated by mean of “iatro-sedation” at USC School of Dentistry, whose Behavior Science Section, under the direction and stewardship of the late Dr. Nathan Friedman, a pioneering periodontist and USC professor of dentistry developed this groundbreaking curriculum in the 1960’s aimed at helping apprehensive patients overcome their fear of dental treatment.
The following essay, based in part on ten years of experience in teaching iatrosedation in the Behavior Science Section at the USC School of Dentistry, is a unique, innovative presentation of this non-pharmaceutical approach to dental anxiety in that it is written from the standpoint of and for the benefit of the patient, rather than the doctor. It is written for dissemination to the general public in the hope that those who have high anxieties regarding dental treatment will know that there is a predictable, evidence-based method by which their fears associated with dental treatment can be dissolved and the quality of their lives can be dramatically improved as a result.
There are many variations of passages of Lorem Ipsum available, but the majority have suffered alteration in some form, by injected humour, or randomised words which don’t look even slightly believable.
i Friedman N. Psychosedation, part 2 –iatrosedation. In McCarthy FM (ed): Emergencies in Dental Practice. Philadelphia, WB Saunders Co. 1979.
ii Friedman N: Iatrosedation. The treatment of fear in the dental patient. J Dent Educ 47 (2): 91-95. 1983.
iii Friedman N. A dentist oriented fear reduction technique: The iatrosedative process. Compend Contin Educ Dent. Vol. X no2 113.
iv Hägglin C, Berggren U, Hakeberg M, Hallstrom T, Bengtsson C. Variations in dental anxiety among middle- aged and elderly women in Sweden: a longitudinal study between 1968 and 1996. J Dent Res 1999;78:1655-61.
v Hakeberg M, Berggren U, Carlsson SG. Prevalence of dental anxiety in an adult population in a major urban area in Sweden. Community Dent Oral Epidemiol 1992;20:97-101.
vi Milgrom P, Fiset L, Melnick S, Weinstein P. The prevalence and practice management consequences of dental fear in a major US city. J Am Dent Assoc 1988;116:641-7.
vii Moore R, Birn H, Kirkegaard E, Brodsgaard I, Scheutz F. Prevalence and characteristics of dental anxiety in Danish adults. Community Dent Oral Epidemiol 1993;21:292-6.
viii Stouthard ME, Hoogstraten J. Prevalence of dental anxiety in The Netherlands. Community Dent Oral Epidemiol 1990;18:139-42
ix Vassend O. Anxiety, pain and discomfort associated with dental treatment. Behav Res Ther 1993;3 1:659-66.
x Corah NL, Development of a Dental Society Scale, J Dent Rest 1969; 48: 596.
xi Janis IL, Psychological Stress, New York, Wiley, 1958.
What is the history of implants? Is it well accepted today?
Four thousand years ago ancient Chinese implanted bamboo pegs into bone to replace teeth. Ancient Egyptians inserted pegs made of precious metals into bone for the same purpose. In 1809 Maggliolo placed a gold cast into the shape of a root and inserted into a socket from which a tooth had just been extracted. (i) After a healing period he attached a tooth to the golden root. In 1887 a physician by the name of Harris repeated the same procedure, but used a platinum post instead of gold. (ii) In the U.S., Edmunds implanted a platinum disc into the jawbone and placed a porcelain crown on top. The long-term prospects of these experimental procedures were not satisfactory. In 1939 Strock published a paper showing that implants made of cobalt-chromium-molybdenum alloy (vitallium) was tolerated well by the surrounding tissues, and is still in use today. (iii)
Between 1939 and 1950’s other kinds of implants were developed and used with varying degrees of success. In 1952 Dr. Ingvar Branemark, an orthopedic surgeon, discovered that titanium cylinders implanted into rabbits fused to the bone. He named this phenomenon “osteointegration,” currently a well-accepted principle in dental implantology. Dr. Branemark then began research into using titanium screws as bone anchors in human beings and accumulated credible data that was not embraced by the scientific community, until 1982. That year the Toronto Conference on Osseointegration in Clinical Dentistry laid down the first parameters of implant treatment. This Conference led to the acceptance of Dr. Branemark’s concept of osteointegration into the dental profession and ushered in the new era of dental implantology.
Today, 4000 years after the ancient Chinese first experimentally used bamboo implants to replace teeth, the dental implant is popular and no longer considered experimental. When proper protocol and guidelines are followed, it is safe and effective according to the FDA. In fact the FDA requires implant companies to furnish enough data from controlled clinical and pre-clinical studies to satisfy the stringent restrictions in order for their product to gain full approval.
Over one million implants were placed by American dentists in 2005. (iv) Successful retention of single-tooth implants, when correctly done, have been reported to be as favorable as 97% over a 5 years period, (v) compared to failure rate of bridges, which reportedly have failure rates as high as 20% within 3 years.

What is an implant?
By the term dental implant, we generally mean a non-biologic (e.g., titanium alloy) post shaped like the root of a tooth that is surgically inserted into the bony ridge (jaw bone) primarily as the (prosthodontic) foundation upon which to build an artificial tooth. (vii) A dental implant generally has two parts. It consists of the root (“body”) and the “abutment”(connector). Separately, an artificial tooth (e.g., crown) is placed over the abutment. The artificial tooth or crown is not considered a part of the implant.
Generally, the body (root) is inserted into the bony ridge and remains submerged under the gum for the prescribed period of healing. At the appropriate time the body (root) is uncovered surgically, and the abutment is then attached to the body. The crown/artificial tooth is then attached to the abutment (connector). In short, the abutment connects the crown to the root (body) of the implant.
Individual results may vary
Are there different kinds of implants?
Yes. There are a large number of types of implants. They are selected by the implant dentist based on many factors, among which are the needs and desire of the patient, the location and condition of the implant site(s), the bite relationship between upper and lower teeth, the general condition of the teeth and gums, medical health and many other factors. But for the sake of simplicity and practicality, all the implants may be grouped into two general categories. The first is the most common and is described in Question 2. It has two parts: body and abutment. The body is placed into the bone and allowed to “osteointegrate” for generally three months. Then the abutment is attached to the body of the implant. A crown or a fixed prosthesis (e.g., fixed bridge) is placed on the implant. This crown or prosthesis is fixed and only be removed by the dentist, not the patient. In this category of implants there are literally thousands belonging to various brands, design, sizes and shapes, along with even more accessory parts. Depending on a particular situation the dentist can choose what is most appropriate for the patient.

The second category of implants is the “instant over-denture mini implants.” This is a one-piece implant that is generally used, with some exceptions, to stabilize removable prosthesis (removable partial dentures or bridgework) and the denture can be “instantly” attached to the denture as soon as the implants are placed. The body and abutment is actually in one piece. But the diameter of the mini- implant is considerably smaller than the traditional implants (1.8mm vs. 4.0mm). The mini-dental implant is shaped like a surgical screw and is affixed into the body by a rotational movement, without incisions. Unlike traditional implants, there is no waiting period. Aftereffects are usually minimal. Thus in one visit the denture patient can walk out of the dental office and immediate enjoy a meal. Unlike traditional implants, mini over-denture implants cannot be used to support fixed prosthesis, such as crowns and fixed bridgework in most instances. Some experienced dentist with in-depth training may be able to employ special techniques to attach crowns to mini implants.
Individual results may vary
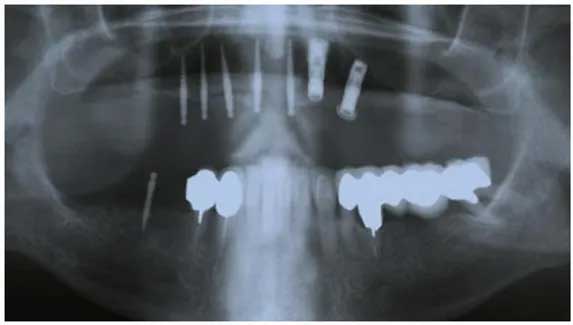
Panoramic View of Upper & Lower Implants
(Illustration of complex case with a combination of Regular & Mini Dental Implants)
Why not get a bridge rather than an implant?
Where an implant is a viable option, “the single-tooth implant represents the treatment of choice from both a health and value standpoint,” according to authoritative sources that have compared the long-term benefits of implants and bridgework. (vi) Some reports sources cite survival rates of bridgework that varies from 3% loss over 23 years to 20% loss over 3 years. Others cite studies reporting 8-12% loss abutment teeth (that anchors the bridge) within 14 years. On the other hand single implant survival rate has been reported by a number of studies to be 94.6 to 100% for 1-15 years. The median of these reports is a 2.8% implant loss over a 5 year period. A review of literature by Goodacre, et al, from 1980 to 2001 found that single implants had a success rate of 97%. (vi, vii)
Implants may not be a viable option in some circumstances. For example, the mandibular nerve is located so close to the surgical site that the risk of nerve injury precludes implant placement without additional surgical procedures, such as bone grafting. The patient’s medical health may also sometimes be a factor, e.g., uncontrolled diabetes.
What are the components of an implant and why is it important for you to know?
There are three items to consider when a tooth is replaced with an implant. The implant itself generally consists of two parts. The first there is the “body” of the implant. This the part that is shaped like the root of a tooth, which is surgically inserted into the bone. The implant body is left under the gum to “osteointegrate,” or fuse with the bone, for a period of time. When healing has taken place (which takes generally 3 months) the implant body is surgically exposed and a second implant part, called the “abutment,” is locked onto the body. Once the abutment is secured to the body, the implant would be ready to be restored by means of a crown or an artificial tooth. Thus there are three elements to be considered when you consider an “implant.” Namely, they are (1) Implant body, (2) Implant Abutment and (3) Crown.
It is important to keep these three elements in mind when you inquire about the cost of an implant. Sometimes the quoted cost of an “implant” is just the expense of surgically placing the implant body into the bone with the understanding that the abutment and the crown are done later and are separately charged. This may be frequently true when the “restorative dentist,” who does not perform implant surgery, refers you to an implant surgeon. The surgeon will only quote the fee for the surgically placing the implant. Your doctor, the “restorative dentist, would give you the estimate for the abutment and the crown. Other times, if your dentist does both the surgery and the restorative part, the quote may be for the body, implant and crown. To avoid misunderstanding, it is advisable for you to ask for clarification and itemization of costs.
Is it always necessary to wait at least three months before the crown is placed on the implant?
No, not always. There are three surgical approaches to implant placement. The first two approaches require a waiting period. The third, called “immediate placement/load” approach, does not require waiting.
(1) The first is a two-stage surgical approach which calls for the body of the implant to be placed into the jaw bone. (Over the implant body a “cover screw” is placed to prevent bone or soft tissue from invading the crest of the body. The (cover screw and the implant body is left to healed submerged under the gum for a period of time, which may be as little (as six weeks or as long as a year. After the prescribed healing period, the implant body is uncovered surgically. The (cover screw is removed. Then abutment is locked and secured onto the implant body by a variety of means. A crown then (can be made to be placed over the abutment.
(2) The second approach is the one-stage surgical approach that calls for the implant body and the abutment to be placed (at the same time. A “healing cap” is placed over the abutment to facilitate proper healing of the soft tissue around (the implant. The abutment and the healing cap are left on the implant body during the healing period and can be seen (projecting above the gum line. No second-stage surgical to uncover the implant is necessary. When healing has taken (place, the healing cap is removed and the crown is then placed onto the abutment. The waiting period may be as short as (six weeks, but could be as long as one year.
(3) Immediate placement calls for the placement of the implant body, the abutment and the crown all the same time. (ix)
The decision whether to undergo immediate or delayed placement is a complex one and should be made by the patient and the doctor after a comprehensive work-up and evaluation of all the risks and benefits associated with the unique circumstances of each case.

What preliminary procedures do I have to go through to get an answer as to whether I can get an implant and how much it would cost?
The dental implant is one of the most reliable procedures in dentistry and is expected to last 20-30 years in most cases. But it also one of the most complex. When appropriate guidelines are followed and all relevant factors are accounted for, the success rate approaches 97% according to some studies. (vii) Therefore it is important that you cooperate with your dentist in carrying out the “pre-implant” evaluation in a comprehensive manner. Some of the factors your implant dentist needs to evaluate are as follows:
a. Review of medical and dental history. Common questions asked include past and present medical conditions and treatment and previous dental treatment. Are there any dental or medical conditions that would preclude an implant procedure? Are there any precautionary (prophylactic) steps that should be taken in consultation with the physician?
b. Diagnostic evaluation and x-ray examination. This step may include the following:
(1) Examining the condition and position of teeth, the smile line, the occlusion bite relationship), location and (dimension of the implant site and other relevant factors. Is there enough space for a implant? Too little space? Too (much? Are there teeth that should be filled first or even extracted?
(2) Examining the soft tissue, which includes the position of lip line, the gum line and the general gum condition. (Does the patient show his/her gum line when smiling or talking? How will the implant procedure affect the smile? Are (the gums in good condition or are there other hopeless teeth that might be lost due to periodontitis gum infection)?
(3) Examining for grinding and clenching habits. Are the existing teeth worn down? Is the patient aware of clenching (and grinding during the daytime or while asleep? Biomechanical force factors exerted against the implants through (clenching and grinding are the leading causes of implant failure. x) What is causing the patient to grind and clench? (Is there a history or obstructive sleep apnea which is associated with grinding and clenching)?
(4) Diagnostic casts. These are duplicates of your mouth made from “impressions” or molds. They allow the dentist to study your teeth and your bite in your absence. Diagnostic wax-up ( mock up of teeth in wax) can be made from these casts. Wax-ups allow the dentist and the patient to visualize what the final result might be and facilitate the selection and placement of your implants.
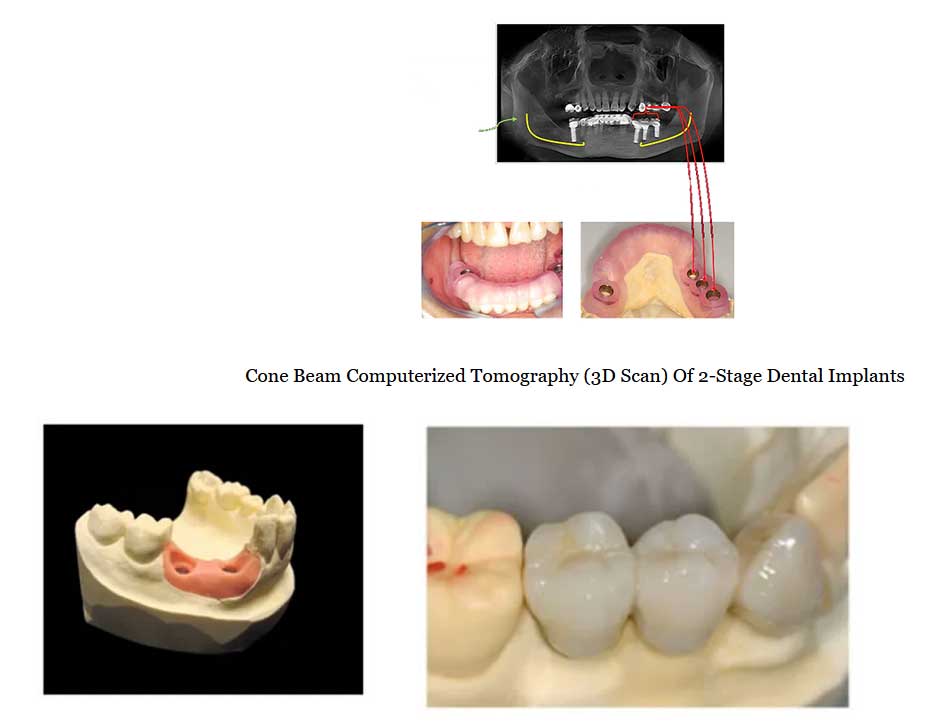
(5) X-rays: digital/film and low-radiation cone-beam computerized tomography CBCT) scan. Traditional two-dimension (x-rays either in the digital or film modality should taken to assess general dental health and general conditions of (the implant site. Additionally, CBCT scan is necessary to ascertain the exact dimension of the implant site as well as (the precise location of the nerves or sinuses close to the implant site. CBCT can help the implant dentist determine (the volume, density and topography of the bone where implant is contemplated. In most circumstances CBCT is essential (to the planning and treatment of the case and the minimization of the risks of surgery.
There have been reports of excessive radiation related to CT scan. Should I be worried about too much radiation from these dental scans (cone-beam CT)?
A recent article published in the New England Journal of Medicine reported that “about one-third of all CT scans that are done right now are medically unnecessary.” This article was referring only to medical CT scans, not dental cone-beam CT scans.
The dose from a dental cone beam CT is approximately 1/10th the dose delivered in medical CT imaging and falls well within the range of doses delivered during conventional dental radiography, according to a joint publication by the Department of Diagnostic Sciences and General Dentistry, University of North Carolina School of Dentistry and Department of Oral Medicine/ Pathology/ Oncology, University of Michigan School of Dentistry. (xi)
Conventional medical CT utilizes a fan shaped beam that images an object slice by slice and then stacks the slices to obtain a 3-D representation of the object. Conventional CT’s are large and expensive and deliver high radiation doses due to the multiple slice acquisition and inefficient use of x-ray photons. They are designed for full body medical imaging and are not always practically available to the dental community.
Cone beam scanners utilize a cone-shaped beam to scan the entire region of interest in a single rotation and are ideal for dedicated imaging of the maxillofacial complex, which lies in the lower two-thirds of the head. The conical volumes of digital information are manipulated by computer software into multiple slices for viewing. This technology not only reduces the size and cost of the scanners, but reduces the inefficiency of x-ray photon used resulting in a considerable reduction of patient radiation exposure. (x)
Even though cone-beam CT scan emits minimal radiation, you should be aware that any amount of x-ray incurs risk to a certain extent. Even exposure to sunlight or background radiation incur some exposure to radiation. After discussing the benefits and risks of an x-ray test with your dentist, the decision to accept the risk with the benefit, or not, is ultimately yours to make.
Once these diagnostic steps have been taken, your dentist will discuss with you the various options available to you. The risks and benefits of the procedures would be explained to you. And at this time it would be appropriate to discuss the costs of the various alternatives.
The cost of replacing teeth with implants depends on many factors, such as the volume and density of bone, location of nerves and sinuses, the condition of the remaining teeth, your occlusion ( bite relationship), habits such as clenching and grinding, and even your own preferences and ability to maintain the implants consistently and regularly. (Read more at Question 6.) Dental plans generally exclude dental implants and CBCT by contract, but will in some instances issue partial coverage for the implant crown. Your dentist may be able to find out whether there will be at least some coverage for the crown. However, in most instances the exact coverage cannot be pre-determined by a phone call.
X-Ray View of 2-Stage Regular Dental Implants
Why do I need to get a dental cone-beam CT?
As compared to traditional x-rays, CBCT has the advantages of having negligible distortion from magnification, relatively high contrast image, various views, three- dimensional bone models and interactive treatment planning (which allows your dentist to do computerized virtual surgery and implant placement in the planning of your treatment)
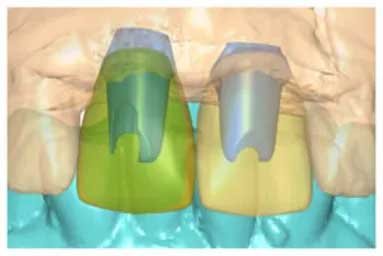
Virtual Surgery via Interactive Computerization (Atlantis VAD™ software)
These properties of CBCT allow, for instance, your dentist to accurately determine in a more precise manner the location of vital structures ( e.g., nerves), quality and dimension of the bone. Furthermore, it allows your dentist to create a “surgical stent” based on the results of virtual implant surgery. The stent guides with high precision the placement of implants into the pre-determined location at the correct depth and with the correct angulation. These advantages enhance the ease of your surgical experience, the long-term success of your case and minimizes risk of complications. It is regarded by some to be the “standard of care” in the planning of implants.
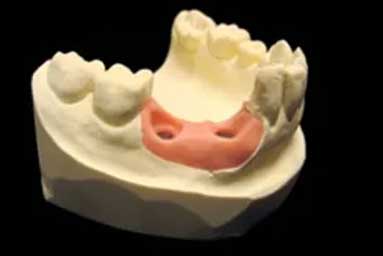
Computerized simulation and planning assisted by surgical stents using CT- Scans allows accurate construction of surgical guides that ensures implant placement without unnecessary risk of complications such as nerve damage or sinus exposure.
What is the cost of a cone-beam CT?
The cost of a CBCT may vary from a low of $250 to $600, depending complexity of the case and special preferences of the dentist prescribing the x-ray.
CT-SCAN OF MANDIBULAR NERVE AS FACTOR IN DENTAL IMPLANT PLACEMENT
Should I consider getting implants at foreign countries or a distant location to save money and perhaps enjoy a vacation?
Yes, you can if you wish. While in some countries there are well-trained dentists who may even charge more, in other countries some dentists would charge considerably less. You may want to consider some confounding issues before you make a decision, for instance:
(1) In considering the cost of implants the patient should keep in mind that it is not just the initial cost of placing the implants and the crowns alone that should formulate your decision. How well will the implant function without complications and how durable the implant will be should also be primary considerations. What is the knowledge, (experience, training and reputation of the prospective dentist in the field of implantology? You are “buying into” something that you would want to last 20 years or more. You expect it to be properly done. You would want to ensure (that necessary steps are taken to ensure success and avoid failure unnecessarily.
Furthermore implants are like real teeth. They must be properly maintained and cared for regularly before they can be expected to last a long time. Your implant dentist must be able to help you maintain your implants on a regular basis. Being in another country or in a distant location may present logistic problems. A dentist in your locality may not be in a position to take up the responsibility to addressing problems with your implants in the absence of background information and availability of implant parts, accessories and instruments.
You need to investigate and discuss these issues with the prospective dentist located some distance from you. Some of these issues can be resolved ahead of time by special arrangement with a dentist located near you, for instance. It is not impossible to make arrangements for exemplary implant work to be done by a reputable dentist in a distant location. Planning in advance will make things work out much better for you in the long run.
(2) Generally implants are done in two stages. The implants are surgically placed into the bony ridge jaw bone) and (left there to “osteointegrate” heal and fuse with the bone) for generally three months. Then you have to return for the (second follow-up procedure. This means you may have to make the trip twice.
(3) On your second trip crowns will be made and placed on the implants. If everything works out perfectly you still need (to return regularly for post-operative maintenance and check-up. No other dentist would be in a position to take (responsibility for these implants. If complications arise while you are there, such as numbness or infection, you may (have to stay in that country for an extended period of time.
(4) If complications arise after you return, the dentist at your home town, if you can find one, would need to contact (your implant dentist in the other country to try to resolve the problem. If the problem is not minor, you will probably (have to make another trip. Major problems would include fracture of implant body or abutment, gum infection, infection (around the implant, TMJ jaw joint) pain, or broken screw that attaches the body to the abutment).
(5) And other issues include matters such as qualification of the foreign dentist, infection control protocol not (necessarily standard in other countries), the brand and quality of implant parts and the availability of these parts in the future.
Is implant surgery very painful? What problems can I expect following surgery?
No, implant surgery is generally not at all painful. Absolute anesthesia can be easily achieved with local anesthetics. Your apprehension is legitimate. Many people ask the same question. However, any past unpleasant experience with dental work when you were younger had to do with teeth that had inflamed nerves, or teeth that were infected. Under those circumstances sometimes discomfort becomes unavoidable. Implant placement involves no natural teeth. Interestingly, bone has no nerves. Placement of implants into bone generally takes place without incident.
Another aspect of implant dentistry that coincidentally reduces post-operative problems is the use of the computer- generated surgical “stent,” or guide. The decision to use a surgical stent designed by virtual surgery through the medium of interactive computerization can make your dental experience much more pleasant. The use of such a stent negates the need to cut or make incisions on your gum. It can be described as a “punch” technique and is relatively quick, as well as precise. Most of the critical work had already been done by your dentist before surgery. That’s why the procedure is generally very smooth. Post-operative symptoms are negligible in most cases.
Generally there may be only mild swelling or mild pain which is taken care of by over-the-counter pain pills. In fact most patients report taking hardly any pain pills at all.
What follow-up appointments are necessary after implants and crowns are done? What are ways to keep implants clean and last long?
What are ways to keep implants clean and last long? Once implants and crowns have been placed, your dentist may need to see you periodically. You may need special instructions as to how to clean your implants. You will probably need to see the dentist or the hygienist for regular cleaning appointments. Special techniques and instruments are needed to clean your implants. Inappropriate instruments may scratch the implants and lead to breakdown of the bone around the implants. Treat your new implants as if they are new teeth. They need good, consistent home care and regular maintenance care at your dentist’s office. Good follow-up care will improve the chances that you can keep these implants and all the rest of your teeth for life.
What causes failure in implants?
Failure of an implant is generally related to the lack of osseointegration of the implant, i.e., fusion of the implant with the bone. Failure to osteointegrate leads to loss of the implant within the first year. Subsequent significant loss of bone around the implant in the following years can also lead to loss of the implant.
The one advantage dental implants have over natural teeth is that they are not susceptible to dental caries (cavities). However, a condition called peri-implantitis can occur. Peri-implantitis is an inflammatory condition of the gums and bone around an implant. This condition may result in loss of bone and eventual loss of the implant. The cause of this condition is unknown and may occur in 5% of the cases. Smokers, diabetics, patients with poor oral hygiene, and cases where the gums around the implant are thin are more prone to peri-implantitis. (xi, xiii)
Can everybody get implants? What are contraindications for implants?
Dental implantology has advanced to the point that almost any healthy person can benefit from implants. However there are some conditions that can present obstacles which must be initially identified and addressed for a case to be successful.
Of particular concern to dental implantologists is the location of the mental foramen and the nerve bundle (neurovascular bundle) that it carries. The mental foramen (hole) is located in the vicinity of the lower bicuspids, near the corner of the mouth. Through this foramen the mandibular nerve in the form of the neurovascular bundle emerges and innervates (gives sensation to) surrounding structures, such as the lip and the cheek. It is critical that the implant surgeon accurately locates the mental foramen and the neurovascular bundle through x-rays and cone-beam computerized tomography (CBCT). Irreparable damage to the mandibular nerve can result in paresthesia (numbness) or dysesthesia (painful numbness) in the chin, lip and face. Sometimes these nerve conditions become permanent and may lead to drooling.
Uncontrolled type II diabetes is a condition that must be corrected before implant procedures are undertaken. Poor peripheral blood circulation may retard healing.
Anatomic problems such as lack of volume and density of bone may be an obstacle. However bone grafting procedures can resolve these problems and should be part of the preliminary evaluation.
Patients receiving intravenous and oral bisphosphonates for osteoporosis or other conditions may be more prone to a condition called “osteonecrosis (bone death). Implants are contraindicated for some patients who take intravenous bisphosphonates.
Bruxism (tooth clenching or grinding) may generate detrimental forces during the healing phase of the implants. After the implants have osteointegrated, the implants are still subject to “micromovements” due to these forces. Over the course of time implants may fail due to these micromovements. The implant dentist may recommend a special device called the biteguard that can minimize this problem. Even with bite guards, bruxism can still can pose a high risk to the longevity of the implant. (xiv)
There are other conditions, although rare, which may impact the viability of implants. This is the reason a thorough preliminary work-up/exam is critical to the predictability of any implant procedure.
What is iatrosedation?
Iatrodedation is defined as an interpersonal-cognitive (doctor-patient) process by which patients sufering from dental phobia are calmed by the behaviors, attitudes, and communicative stance of the dctor. (i,ii) It is non-pharmaceutical. It is effective particullarly in treating dental fears that originate as a consequence of one or more traumatic conditioning experiences. (iii) Thousands of dental patients with dental phobia or high anxiety levels have been successfully treated with iatrosedation at Herman Ostrow School of Dentistry of USC since the 1960’s. This proven fear dissolving therapy, for the most, is accomplished without the use of pharmaceuticals, such as general anesthesia, IV sedation or oral medication. After having treated thousands of highly anxious patients over twenty-five years I have observed that the dissolution of phobia, without pharmaceuticals, becomes a mark of personal triumph and empowerment that reverberates through the personality of the patient in astonishing and remarkable ways.
What is dental phobia?
A phobia is an intense and persistent fear of certain situations, activities, things, animals, or people. The main symptom of this disorder is the excessive and unreasonable desire to avoid the feared subject. (ii) Dental phobia may be described as excessive and unreasonable fear of dental treatment.
How is dental phobia different from other phobias?
In contrast to many other phobias, sufferers subject themselves to regular and repeated exposure to threatening stimuli, or may be expected to do so. Dental phobia, compared to other specific phobias, avoiding the feared situation in many cases leads to significant negative conse¬quences. For the truly phobic individual, it is com¬mon for a vicious cycle to develop in which fear leads to avoidance of dentists, resulting in neglected den¬tal care, increased awareness of these unmet needs, and feelings of shame. These factors give rise to nega¬tive social effects and hence to increased anxiety, (iii) not to mention the added financial burden of deferred dental care.
How prevalent is dental phobia?
Up to 40 percent of the adult population admits to being fearful of dental treatment, of which 3 to 5 percent can be said to be truly phobic or to have a debilitating high level of fear. (iv v vi vii viii ix) It is estimated that at least 20 million Americans suffer from dental phobia. (i)
How can I know how severe my condition is?
There is The Corah Dental Anxiety Scale, developed in 1969, by Dr. Norman L. Corah, from the Department of Behavior Science, School of Dentistry, State University of New York, (x) that can help you assess your anxiety level. Fill out the following questionnaire then follow instructions on how to score this test.
1. If you had to go to the dentist tomorrow, how would you feel about it?
a. I would look forward to it as a reasonably enjoyable experience.
b. I would NOT care one way or the other.
c. I would be a little uneasy about it.
d. I would be afraid that it would be unpleasant and painful.
e. I would be very frightened of what the dentist might do.
2. When you are waiting in the dentist’s office for your turn in the chair, how do you feel?
a. Relaxed.
b. A little uneasy.
c. Tense.
d. Anxious.
e. So anxious that I sometimes break out in a sweat or almost feel physically sick.
3. When you are in the dentist’s chair waiting while he gets his drill ready to begin working on your teeth, how do you feel?
a. Relaxed.
b. A little uneasy.
c. Tense.
d. Anxious.
e. So anxious that I sometimes break out in a sweat or almost feel physically sick.
4. You are in the dentist’s chair to have your teeth cleaned. While you are waiting and the dentist is getting out the instruments which he will use to scrape your teeth around the gums, how do you feel?
a. Relaxed.
b. A little uneasy.
c. Tense.
d. Anxious.
e. So anxious that I sometimes break out in a sweat or almost feel physically sick.
How to score this test: Add one point for each “a.” Add two points for every “b.” Add three points for every “c.” Add four points for every “d.” Add five points for every “e.” Total scores can range from 4 – 20. Average score is 8-9 and a high score typical of a dental phobic would be 17-20. (In one sample of 1,232 college students the mean score was 8.89, with a standard deviation of 2.99, whereas the median and mode were both 8.) (ix)
These scores are not diagnostic of your condition. Obviously a high score would suggest a need to look further into the possibility that you have a high level of anxiety or fear toward dental treatment. No matter what the score is, it is advisable for you to share the result of this test with your dentist.
How does an individual become dental phobic?
Dental phobia may be described as excessive and unreasonable fear of dental treatment. The patient needs to consciously acknowledge that this fear is learned as a consequence of direct or indirect experience, and is not a congenital condition that should be accepted as immutable. A direct experience may be associated with a traumatic encounter in a dental office or a medical procedure. Even the memory of an experience not related to dentistry or medicine, e.g., a near-drowning experience, may be brought to reminiscence by dental treatment.
An indirect experience is one in which the fear is learned vicariously. Generally this is experienced through stories told by the parents or siblings, or observation of the after-effects of dental procedures. Other medium, such as TV and movies, may also be conditioning factors.
These experiences most frequently occur during childhood, although feelings associated with the memories may persist throughout life. Fortunately the ability to “unlearn” this “neuro-cognitive pattern” is resident in every individual.
You mentioned how one can "unlearn" the pattern of fear. But how does one "learn" dental phobia in the first place?
One “learns” fear through a phenomenon called “classical conditioning.” Heightened fear of dental treatment can be described as a “conditioned response,” in a sense similar to the response in “Pavlovian classical conditioning.” Pavlov observed salivation (unconditioned response) when food was offered to the dogs. Then he rang a bell every time food was offered. Soon the dogs salivated (conditioned response) simultaneously with the sound of the bell.
Similarly, when a child experiences pain from a needle or drill, he/she associates the dentist with pain. The fear of the dentist then becomes the conditioned response and whenever he/she thinks of the dentist or actually goes in for a dental appointment it translates into fear.
This conditioned response may generalize from the original traumatic circumstances to other situations. For example, fear of injections for immunization or antibiotics may be generalized as a response to dental injections, or vice versa.
Conditioned responses may also be learned through “modeling.” Parents sharing their traumatic experiences with their child become a modeling experience for the child. The child learns a “conditioned response” as a result. Parents can ingrain the fear response by comments such as, “If you don’t behave, I’ll take you to the dentist.” No wonder the child becomes wild with fear at the dental chair. The child can also learn to fear dental treatment through the medium of television or movies.
You mentioned how one can "unlearn" the pattern of fear. But how does one "learn" dental phobia in the first place?
One “learns” fear through a phenomenon called “classical conditioning.” Heightened fear of dental treatment can be described as a “conditioned response,” in a sense similar to the response in “Pavlovian classical conditioning.” Pavlov observed salivation (unconditioned response) when food was offered to the dogs. Then he rang a bell every time food was offered. Soon the dogs salivated (conditioned response) simultaneously with the sound of the bell.
Similarly, when a child experiences pain from a needle or drill, he/she associates the dentist with pain. The fear of the dentist then becomes the conditioned response and whenever he/she thinks of the dentist or actually goes in for a dental appointment it translates into fear.
This conditioned response may generalize from the original traumatic circumstances to other situations. For example, fear of injections for immunization or antibiotics may be generalized as a response to dental injections, or vice versa.
Conditioned responses may also be learned through “modeling.” Parents sharing their traumatic experiences with their child become a modeling experience for the child. The child learns a “conditioned response” as a result. Parents can ingrain the fear response by comments such as, “If you don’t behave, I’ll take you to the dentist.” No wonder the child becomes wild with fear at the dental chair. The child can also learn to fear dental treatment through the medium of television or movies.
Does the doctor using the iatrosedative approach have a different take on the doctor-patient relationship when it comes to highly fearful patients?
Fearful patients require a specific kind of behavior from doctors, according to Dr. I.L. Janis, who conducted an extensive five-year study of psychological stress endured by patients preparing for and undergoing major and minor surgery, including operative dentistry. (xi) This study determined that doctors have a powerful influence on the patients’ fear and stress levels. Patients perceive the doctor in two important ways:
1. A Danger Control Authority.
2. A Protective Authority.
The doctor controls what the patient perceives as dangerous and is the one who can protect him from that danger. Because of this perception the doctor’s behavior and mannerism assume great significance in the mind of the patient. The patient is looking to the doctor to protect him/her from danger. This takes place through an interactive two-way dialogue (iatrosedative interview) during which a process takes place that results in the patient developing trust and confidence in the protective authority of the doctor. Having built up trust, the patient then can better cope with the stress of the surgery.
For this reason the doctor needs to find out during the iatrosedative interview:
1. What do you perceive as threatening or dangerous?
2. What can the doctor do to make you feel safe and protect from the danger?
How can I prevent my children from getting dental phobia, like I did?
You can apply the initial steps of the iatrosedative method to alleviate your child’s anxieties regarding dental treatment. You should consider doing the following:
• Be positive yourself regarding dental treatment at all times. Sometimes that is all you need to do to instill confidence and trust of the child toward the dentist. Do not engage in negative talk about dentistry in front of your children.
• You should take your child for a routine checkup when she/he is two years old, according to the American Dental Association. This will allow the child to be comfortable with the dental environment and the doctor and the staff.
• If your child is especially fearful or anxious, acknowledge your child’s fear as real, whether you believe it is justified or not.Accept your child’s fear and anxiety with understanding and empathy.
• Talk to your child about the possible sources of the anxiety/fear. Was there an unpleasant experience with a dentist? With a medical procedure? Did the child hear or see something that was frightening? Did the child adopt this anxiety vicariously from another member of the family?
• What specifically caused the fear/anxiety? The sight of the needle, the injection, the numbness, the bad taste of the anesthetic, the noise of drill, the tooth still hurt after injection, fear of the white coat, etc.
• Reassure your child you will see to it that this would not happen again. You might even visit the office and get an “office tour,” say hello to the doctor and perhaps ask some questions as to what the doctor thinks you should do to reassure your child. Then you have strong personal basis to reassure your child.
• During the office tour, you can inquire as to how the doctor handles difficult pediatric cases. Does the doctor typically use pharmacosedation? What medicine is used and what are its side effects? Does the doctor discourage or permit the presence of the parent in the operating room? Can you be there when your child comes out of sedation so that the child wakes out in your reassuring presence? Does the doctor typically use restraining devices, such as the papoose? How do you feel about restraining devices for your child? Does the doctor typically use iatrosedation, with no physical restrain or pharmaceuticals? This would be the best, if it is practicable for your child.
• You should book an appointment first thing in the morning, if possible. Be sure your child has gotten a good night’s sleep and a healthy breakfast. Your job is to make sure your child is happy at the first appointment.
• When you talk to the doctor about what is needed, give serious consideration to talking to the doctor away from the child. You can then share with the doctor your concerns and that of your child’s. Questions such as, “Should I stay with the child during the procedure?” How does the doctor treat an anxious child, such as yours? What pharmaceuticals, if any, will be used? You may discuss the possibility the pharmacosedation may be needed, at least in the beginning.
• You may reassure your child with positive reinforcement and strongly, positively express your trust and confidence in the doctor.
• When the appointment is over, praise your child regardless of how the appointment went. Smile when you see your child. Do not show a face that says, “ Poor baby, it might have been terrible.” Say something like, “I am so proud of you.” The doctor/nurse said you did great! You will be pleasantly surprised at how happy your child will be the next time.
What is the process I need to go through to overcome this phobia?
A. This question will be answered in three parts. The first part consists of you doing some thinking about the problem before your first appointment.
1. You must recognize and accept the fact that you have an inordinate fear of dental treatment. Twenty million other adults have the same condition. You learned this conditioned fear response through no fault of your own. You have nothing to be ashamed of, nor to feel guilty about. It’s OK for you to be a “dental coward,” or “dental chicken.” Some of the bravest people, including decorated veterans, are also afflicted with this condition.
2. You might want to give thought to the following questions, if it doesn’t bother you too much.
• What exactly are you most afraid of? For example, is it the injection? Is it the fact that it wasn’t numb enough? It is the noise? The smell? Is it the numbness? Do you feel claustrophobic in the dental chair?
• Can you associate that with some experiences in the past? Was it an experience related to a dental appointment? Or a medical procedure? Was it a series of dental or medical experiences? Was it something that was not at all related to any dental or medical procedures?
• Was your fear response learned some other way, e.g., through you parents or siblings? Now that you have recognized, accepted and have some idea as to how you acquired dental phobia, you are now ready for your first meeting with the doctor.
B. Your first visit with the doctor is called the Iatrosedative Interview. This interview may proceed in different ways, but generally will move along in four segments.
1. You can expect that the doctor will verbally and non-verbally communicate understanding and acceptance of your expression of anxiety or fear. The doctor is well aware that fearful patients are very perceptive and sensitive to the doctor’s behavior and will do everything possible to reassure you.
2. The doctor will explore and identify the problem through the use of questioning and facilitation skills to determine:
• The specific fear and its intensity.
• The origin of the fear.
• The behavior of the doctor(s) or authoritative figure(s) that may have been involved in the traumatic conditioning that occurred.
By determining the specific fear and its origins the doctor will be better able to offer a specific solution and formulate a plan that would help you, the patient, to “un-learn” the conditioned response.
3. The doctor will explain his interpretation of your unique circumstance:
• How your fears were learned, whether this is apparent or not.
• How fears may be associated with helplessness, dependency and the unknown. The doctor may discuss with you the different ways in which you can exert control over your treatment and that you will participate in the choice of treatment, and have control during the treatment itself, such as stopping the procedure at any time. Having control over treatment will help alleviate feelings of helplessness and having knowledge of the treatment will help relieve the fear of the unknown.
• How you have the ability to unlearn the sense of danger and relearn a sense of safety. The doctor may share with you how other patients just like you have also relearned under his/her care.
4. The doctor will offer a solution to the problem:
• How the doctor will perform the procedure in a way that will bring about a totally different result.
• What kind of behavior the patient can expect from the doctor, such as taking every precaution to make the injection as painless as possible and that the tooth will have “absolute anesthesia” before procedure is begun.
• Offer of control so that the treatment will be stopped if the patient feels the need. The doctor may assure the patient even if the patient does not complain, the doctor will know through experience and observation when to stop and inquire.
• Patient will be kept informed as to what to expect as the treatment progresses (Preparatory communications).
• The doctor will keep a two-way line of communication open to the patient to answer questions or discuss the patient’s state of mind.
C. Iatrosedative Clinical Appointment. This is the appointment during which a dental procedure will be done for you. This is what you may expect the doctor to do to help you “relearn” the condition response of fear and anxiety:
1. Preparatory Interview: this is a brief two-way dialogue concerning the anticipated procedure. The doctor will want to find out two things:
• Have you ever experienced this particular procedure before?
• How do you feel about it?
The reason for this inquiry is to prepare you for the details, such as the kind of instruments to be used, so that potentially threatening perception of danger can be avoided and the doctor can take steps to make sure this time things will work out much better than the past.
2. Nonverbal Empathic Behavior. Without words the doctor exhibits these following traits:
• Attentiveness and concern.
• Acceptance of you and your problem.
• Supportiveness.
• Involvement with the intent to help.
3. Physical attending skills. The experienced doctor will naturally exude the following characteristics:
The words that the doctor uses will be augmented with good eye contact, forward trunk lean, good body orientation and good distance so that the intent to communicate empathy is accomplished.
The experienced doctor is well aware that facial expression needs to convey warmth, interest and concern so that the words spoken will have the intended impact.
The voice is an important instrument in helping the highly anxious patient to relax and feel safe and protected. Generally the doctor will speak with moderate volume, pitch and resonance, such that the voice is consistent with the words and facial expression.
At the conclusion of the iatrosedative encounter you will have made significant progress in “unlearning” the neuro-cognitive response that has haunted all you life and relearning that dental treatment can be a pleasant, enjoyable experience surrounded by your doctor and staff who care about you.
How can I find a dentist that will help me "un-learn" this fear pattern?
It would be best if you can find a doctor who is trained and experienced with the iatrosedative approach. At the present there are no formal lists of doctors who by training, knowledge and experience are specially positioned to take care of phobic or highly anxious dental patients. However, it can be assumed that many graduates from the USC School of Dentistry have been trained in this method. Your inquiry may consist of whether the doctor you have been referred to is trained and experienced with this method.
It should be said that many dentists intuitively incorporate the principles of iatrosedation into their chairside manner and can attend to the needs of the highly anxious patient with predictable success. The best way to find someone like this is through word of mouth. You need to find a person with similar anxiety levels as you and who has been successfully treated by a doctor. You may ask your friend how the doctor was able to help him or her.
Once you have been given such a referral you may call the office and talk to the receptionist or office manager. Be frank and explain what your condition is and ask whether, in the opinion of the staff, whether this doctor is particularly suited to treat you. Feel free to tactfully ask for the doctor’s familiarity with the iatrosedative method or other non-pharmaceutical means of treating dental phobia or high anxiety. When you meet the doctor, feel free to be completely open about how you feel and what you expect the doctor will do for you. The experienced doctor will welcome such open communication and will be better able to help you.
Why shouldn't I just get "knocked out" for whatever dental treatment I need?
Pharmacosedation is the medical terminology for being “knocked out” for a surgical procedure. It includes oral sedatives, nitrous oxide (laughing gas), IV conscious sedation and general anesthesia. Pharmacosedation is effective in enabling the highly fearful patient to receive needed urgent dental treatment. Apart from the cost of pharmacosedation, the disadvantage with this method is that the source of the anxiety is never dealt with. The phobia still dominates the life of the sufferer as it did before. It would be difficult for the patient to return regularly for maintenance care. What is most lacking with this method is that, because of the high level of anxiety, the patient may find it difficult to communicate with or bond with a particular doctor and his staff.
However pharmaceutical sedation as a means to reach the of goal of iatrosedation is an acceptable, and sometimes necessary method, for helping patients with high levels of fears and anxiety. It is debatable whether long-term dependency on pharmaceutical sedation alone without addressing the underlying causes of anxiety is necessarily the best course of treatment for all anxious patients.
Remember also that overcoming this phobia will empower you to live a better life in ways that you may not have considered before. Having a wonderful smile, with you teeth well taken care of, will likely give you an incredible sense of well-being and heightened self-regard.
If you feel a combination approach will help you, do not hesitate to discuss this with your doctor.

